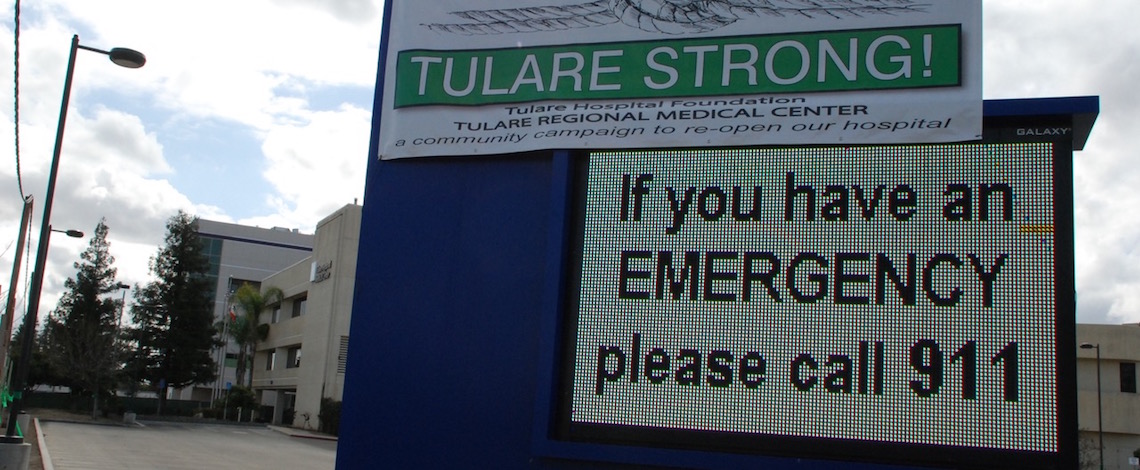
May 2018 file photo of Tulare Regional Medical Center
Written by
Allegations and testimonies are coming to light about the sharp decline in medical care that was experienced at Tulare Regional Medical Center while under Healthcare Conglomerate Associates’ control—a decline that reportedly played a part in the endangerment and deaths of patients.
Among the claims is insufficient equipment that was breaking down and in need of repairs. Due to the hospital’s poor credit from failing to pay its vendors, however, they were unable to replace it. This was the experience of Dr. Lonnie Smith. A nose, ear and throat doctor, Smith worked at TRMC from 1994 to 2016 and served on the Tulare Local Healthcare District Board of Directors from 2006 to 2012.
One common problem encountered was with the oral suction machine in the hospital important to his practice.
“The wall-mounted one—the one that was actually in the wall—that would go at times, sometimes during a case,” he said. “Sometimes in my cases, three or four times, we would have to boot up the new portable suctions to take their place.”
Dr. Smith reported that he was forced to call off and reschedule cases with patients due to missing parts in some cases. Though Dr. Smith did not experience it, other reports have emerged claiming that equipment was taped together, according to Citizens for Hospital Accountability in Tulare.
High turnovers and skeleton crews
TRMC also suffered from severe staffing problems. The hospital dealt with high turnover rates, resulting in a revolving door of new technicians and nurses. This meant training and teaching the assistants, which proved to be a time-consuming process for those involved.
“They wouldn’t know where things are because they’re learning—they’re brand new,” Dr. Smith said. “You have new scrub techs and they didn’t know your routine and what you use, so you have to start over again, step-by-step and teach them how you get things done and how you get the tray set up, how you perform the operation and how they’re supposed to help you.”
Further problems were encountered by other surgeons and staff working overtime. This was reportedly due to bare minimum numbers of people.
“They would start the cases late in the evening, late in the afternoon and have a skeleton shift, you have just your emergency people around and they would try to get the cases done in three or four hours,” Smith said. “It might take them five hours because now you’re with short staff, you don’t have everyone there that helps with things that need to be done, patients need to be moved.”
Patient deaths
Poor equipment and staffing issues may have been key factors in the deaths of two patients to come through the doors of TRMC, according to a finding by the California Department of Public Health.
Among the findings of the investigation was the claim that patients were wheeled out mid-surgery to work on other cases because of the lack of operating room personnel. One of the more publicized deaths was that of Christine Griesbach, 67, who was taken to TRMC in September 2016 for abdominal pain. Griesbach waited for nearly 14 hours in the emergency room, but never made it to the operating table. Her condition declined and she died while waiting.
Faulty equipment may also have been a factor in her death.
“The nurses realized her blood pressure’s failing, but they’re thinking the blood pressure machine’s not working, because that’s typical,” said Patricia Drilling of Citizens for Hospital Accountability. “It must have happened all the time, but it wasn’t even put back on. There were a lot of errors in that, but the bottom line is their way of thinking is: ‘Oh, that must not work.’”
The state report also found that one patient had a surgical tool left inside of him or her.
Another case from 2015 that resulted in the death of an unborn child led to a malpractice suit against TRMC attending physician Rebecca Zulim.
According to records at the Tulare County Superior Court in Visalia, plaintiff Kristen Brown went to the hospital and received a hemorrhoidectomy when she was pregnant. In the complaint, it was stated that the procedure was “negligently and carelessly performed”.
The complaint further alleges that Dr. Zulim “intentionally misrepresented the necessity of the hemorrhoidectomy as it was not medically indicated and highly dangerous during pregnancy.”
Dr. Zulim, it was claimed, knowingly concealed the risks and nature of the procedure and only performed the surgery to obtain a fee, as the surgery was unnecessary. Dr. Zulim denies any wrongdoing or error on her part.
“I had experts review the case and they did not think that I was at fault for the death of the fetus, or that I had committed malpractice,” Dr. Zulim said.
Dr. Zulim stated that further questions should be forwarded to her attorney, Michael Mordaunt in Stockton. The Business Journal reached out to Mordaunt’s office, but has not heard a reply.
Richard Watters, Brown’s attorney in the case, said that the two parties settled the case in 2017 for a confidential amount.
Dr. Zulim was later named surgery chair at TRMC.
Firing the MEC
According to Citizens for Hospital Accountability and Dr. Smith, the practices occurring at TRMC eventually came under the scrutiny of the medical executive committee (MEC) for the hospital. The solution to this problem was reportedly to fire the MEC In January 2016.
“A lot of these people they put in charge were people who had problems with the MEC, either because of quality issues, patient issues, that they now said: ‘Well, we’re going to fire those people and put you in charge,’” Smith said. “They took these people because they knew they could control them.”
The new MEC put in charge resulted in provisional status for the doctors, Dr. Smith being among those who saw it as the last straw.
“’Provisional’ is when you first come to a hospital, they don’t know much about you,” he said. “So they don’t give you voting rights, you have to be proctored—that was a huge slap in the face.”
As a result of the replacement, TLHCD board member Dr. Parmod Kumar ended up being one of the new MEC members, along with his wife, Dr. Parul Gupta.
A member of the Board of Directors from 1994 until his recall in 2017, Dr. Parmod Kumar was an outspoken supporter of HCCA from the start of their bid for management and at a special board meeting on Dec. 5, 2013, was one who motioned for the hospital to enter into negotiations with HCCA. Credited by many as critical to the takeover, Kumar has been by critics as the company’s inside man in the board.
“Kumar’s really good at figuring out what somebody needs and then they get beholden to him,” Drilling said. “And he’s very charming.”
Dr. Kumar’s support of HCCA also seems to have had its benefits—he was appointed medical director for the Southern Inyo Hospital in Lone Pine, another facility run by Dr. Benny Benzeevi’s company. This position reportedly came with a $7,500 charge per two-hour visit. He also gained a reputation for how he billed TRMC for his work.
“He would come in at 11:55 p.m. and he would leave at 12:05 a.m. and he would charge two visits,” Drilling said. “Same visit, but two different days.”
Dr. Kumar’s support for the company also allegedly helped with his appointment to the MEC. With the new committee at the helm, however, critics say that the hospital lost whatever accountability it had left.
“These are the people they put in charge. They were now running the department,” Dr. Smith said. “Handpicked by the Board and with the help of Dr. Kumar.”
The Business Journal reached out to Dr. Kumar’s office, but he declined to comment.








